Natural Treatment of Endometriosis in Benin
- By rachi23
- On 14/11/2023
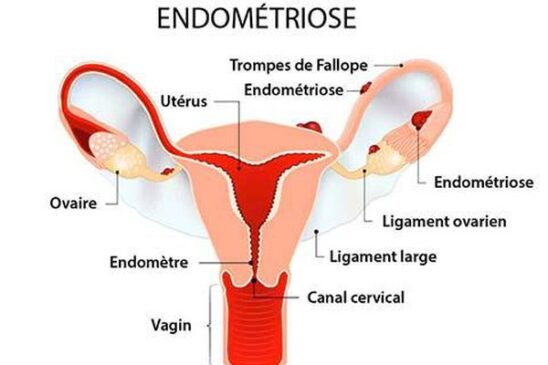
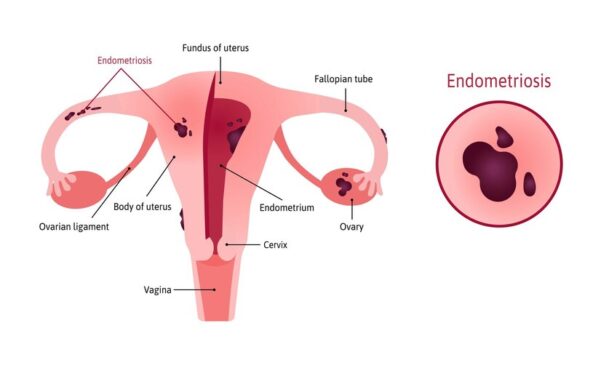
Endometriosis is a chronic gynecological pathology. This disease is characterized by the formation of tissue similar to the uterine lining outside the uterus. Furthermore, as symptoms endometriosis manifests itself by pain in the lower abdomen, accentuated during menstruation, and infertility problems.
For better healing we offer you a very good natural treatment produced in Benin made from leaves and roots. Read until the end to find out.
Please contact us at http://wa.me//+22967546677
Written and edited by DJIMA Rachidatou on 11/14/2023
Make an appointment with a specialist at
Related search
Which plant to use for endometriosis?
How to calm endometriosis without medication?
How to get rid of endometriosis?
How to treat endometriosis in women?
Is it possible to get pregnant with endometriosis?
What makes endometriosis worse?
Definitions And Symptoms Of Endometriosis
Endometriosis is a benign, chronic inflammatory disorder that spreads like cancer but very rarely degenerates into cancer (less than 1% of cases).
Definition of Endometriosis
Endometriosis is a disease in which fragments of the lining of the uterus (endometrium) or ‘endometrial tissue’, including glands and stroma (tissue that supports, protects, and connects together nerves, blood vessels, and lymphatics within the uterus), are present outside the uterus. Endometriotic lesions have the same characteristics as the lining of the uterus. In particular, they are sensitive to the action of ovarian hormones (estrogen). This is why endometriosis is called an ‘estrogen-dependent disease’.
 L’endométriose se
L’endométriose se
This occurs in women of childbearing potential (when the child is physically active), sometimes as early as adolescence. It is a chronic disease that regresses at menopause.
Please contact us at http://wa.me//+22967546677
THE LOCATION OF ENDOMETRIOSIS LESIONS
Most often, endometriosis lesions are present in the pelvic region or pelvis at the following:
- ovaries (endometriomas);
- the peritoneum;
- uterine ligaments;
- the rectum (the septum between the vagina and rectum);
of the bladder.
Less commonly, they are outside the pelvis at the level of
the colon or small intestine;
cervix, vagina or vulva;
the inner abdominal wall (toward the umbilicus, the bottom of the groin, or in an area with scars)
ureters (tubes connecting the kidneys to the bladder);
omentum (fold of peritoneum).
Rarely, endometriosis can develop in organs far from the uterus (such as the pleura and lungs).
Multiple organs may be affected in the same woman.
What is adenomyosis?
Adenomyosis is when endometrial fragments are abnormally present inside the uterine muscle (or myometrium) either diffusely or focal.
Adenomyosis may or may not be associated with peritoneal endometriosis.
Please contact us at http://wa.me//+22967546677
FACTORS THAT CONTRIBUTE TO ENDOMETRIOSIS
Endometriosis develops when several factors are present at the same time (called multifactorial). According to the researchers, it occurs mainly during periods, because fragments of the endometrium move up the pelvis through the fallopian tubes (‘retrograde menstruation’). These pieces of mucous membrane would then attach themselves outside the uterine cavity, to the peritoneum or to the organs.
Other promising elements have been identified:
- mechanical problems that can block the genital system (e.g. cervical abnormalities);
- a genetic predisposition (family risk of developing the disorder);
- hormonal factors (lesions are hormone-dependent);
- an inadequate immune and inflammatory response by the body, leading to the development of lesions.
It is also known that the risk of having endometriosis is increased in
women who have not had children;
those who have short menstrual cycles and heavy menstrual periods.
In contrast, women using oral contraceptives have a lower likelihood of having one.
Before talking about treatment, what are the symptoms to treat?
First, endometriosis is rarely cured. The disease may be "paused" during pregnancy and usually stops at menopause (unless synthetic hormones are continued).
Each patient may have different symptoms. They will depend on the areas where the endometrial cells are located (genital, digestive, urinary or pulmonary apparatus) and on the extent of the lesions caused by their bleeding at the time of menses (scar tissue, adhesions, cysts, etc.). In addition, it is quite possible to be affected without having apparent symptoms (25 to 50% of cases).
SYMPTOMS OF ENDOMETRIOSIS
Endometriosis may not be recognized and may not impair fertility. In some cases, endometriosis is painless but affects fertility. The diagnosis is then made during an infertility evaluation.
When symptoms are present, pain predominates. However, its intensity does not correlate with the extent of endometriosis damage.
The pain of endometriosis
Endometriotic pain occurs mainly in the pelvic area (the lower abdomen) but also in the abdomen and lower back and is often punctuated by menstrual cycles and may result from
- endometriosis lesions themselves;
- invasion of nerves by these injuries;
- inflammatory body reactions;
- fibrous and scarred adhesions that sometimes develop between affected organs.
Sometimes pain is constant. However, in most cases, they are recurrent, punctuated by the menstrual cycle, more marked at the time of ovulation and especially of the menstrual periods (dysmenorrhea or painful periods).
These pains are:
- often strong (poorly controlled with acetaminophen and nonsteroidal anti-inflammatory drugs),
- interfere with daily activities, cause absenteeism from work,
- become more pronounced over time.
Their intensity is related not to the volume or size of the lesions but to their depth of penetration into the wall of the organs. Pain can also occur with changes in position when deep injuries are sustained.
Finally, deep pain may be felt during sexual intercourse (dyspareunia).
Please contact us at http://wa.me//+22967546677
Painful periods in adolescence
Pain during menstrual periods in adolescence after puberty may be the first symptom of endometriosis.
Talk to your doctor about this during the follow-up medical evaluation between 15-16 years of age.
Other symptoms related to endometriosis
Various symptoms are also possible depending on the location of the endometriosis and are usually more intense during menstrual periods.
Urinary symptoms
Pain and discomfort when (dysuria) may develop if the urethra is affected.
If endometriosis is damaged in the bladder, blood may be present in the urine (hematuria).
Digestive symptoms
Pain during defecation (dyschezia) or painful tension of the anal sphincter (tenesmus) as well as blood marks during stool passage occur when the recto-vaginal septum is damaged.
Natural Treatment Of Endometriosis
Natural solutions
Several plants can help with hormonal regulation. Endometriosis is an estrogen-dependent condition, meaning that it is stimulated by estrogen, one of our female sex hormones. Therefore, estrogen-lowering therapies may help slow the progression of lesions and relieve symptoms and signs. On the same principle, phyto-hormonal treatment consists in continuously giving plants with strong anti-estrogen activity.
The Center Afrique Santé Bio (ASB) provides you with a natural cure treatment for endometriosis. It's a very effective treatment. The patient survives for 3 months. After these three months, the patient can go and do a test again so that the center can know what treatment to give.
CLICK HERE TO FIND OUT ABOUT THE TREATMENT
This herbal treatment must be completed with a comprehensive management. The problem must be addressed as a whole: alleviating pain, reducing the frequency and amount of bleeding, slowing ovulation, and relieving psychism. For example, I always prescribe magnesium and vitamin B6.
I advise to use therapies that act on the neuro-psychic component (anxiety, depression), venous and lymphatic circulation, pelvic congestion or digestive disorders. My suggestions: general and gynecological osteopathy, the Mézières method, lymphatic drainage, acupuncture and traditional Chinese medicine.
Alternative Medicine
If the combination of these natural treatments can relieve patients, chemical and/or surgical treatments may sometimes be needed. I am thinking, for example, of infertility situations, where accepting heavy treatments for endometriosis may prevent the use of (even more burdensome) assisted reproductive techniques.
Consultation with a specialist remains essential.
Make an appointment with a specialist at
EVALUATION FOR ENDOMETRIOSIS
Because endometriosis is often diagnosed late, it may take several years from the first symptoms until the diagnosis is confirmed.
The attending physician evaluates the nature and extent of the pain symptoms. If needed, they refer the woman to a gynecologist or gynecologist-obstetrician, who examines her for suggestive findings. Occasionally, these findings are completely normal, but the diagnosis of endometriosis is not ruled out.
To help refine the diagnosis, doctors may do certain tests.
Ultrasonography of the abdomen and pelvis
Ultrasonography of the abdomen and pelvis can show endometriosis.
To better detect some endometriosis injuries, pelvic ultrasonography is done transvaginally (the ultrasound probe is placed in the vagina, so high-quality images can be obtained).
Endometriosis: When is MRI useful?
MRI is prescribed for the following:
- check the peritoneum or viscera (rectum, vagina, uterus, bladder, ureter, small intestine, etc.) for endometriosis;
- define their number and location before possible surgical treatment.
Other tests depending on the location of endometriosis
If colon involvement is suspected, a colonoscanner may be done to accurately record digestive tract injuries. Coloscanner is done by doing an abdominal-pelvic CT scan after the colon is filled with water by placing a cannula in the rectum. This well-supported examination requires no special preparation.
Endoscopic ultrasonography of the rectum, done by a gastroenterologist, may be needed if there is damage to the digestive tract. It allows the digestive tract of the rectum and sigmoid to be seen very precisely up to 40 cm from the anus.
If necessary, if urinary endometriosis is suspected, specialized advice is sought and a urinary tract evaluation (renal ultrasonography, MRI urography, etc.) is also planned
The Place of Laparoscopy in Endometriosis
Laparoscopy is considered only in certain cases. It is used to explore the pelvic and abdominal cavity and identifies the following:
- endometriosis lesions (number, location);
- possible fibrous and scar adhesions.
This test also allows endometrial tissue to be removed from the lesions, analyzed, and confirmed (called a pathologic examination). At the same time, it usually removes visible damage (therapeutic phase).
Laparoscopy limits the opening of the abdominal wall. This technique begins with making four small incisions to inject gas into the abdominal cavity. Then, the surgeon inserts surgical instruments and a miniature camera through the openings into this space. This allows her to operate by monitoring her gestures on a video screen.
After the evaluation, a review of organs affected by endometriosis
The balance sheet shall be used to define:
- adenomyosis: the location of endometriosis in the muscle of the uterus,
- superficial endometriosis localized only to the peritoneum,
- ovarian endometriosis,
- deep endometriosis with or without digestive tract involvement.
Please contact us at http://wa.me//+22967546677
HOW ENDOMETRIOSIS PROGRESSES
Endometriosis is a chronic disorder that develops throughout a woman's period of genital activity. Thus, with each menstrual cycle, the sores proliferate, bleed, and leave fibrous scars.
With treatment, symptoms lessen and the damage resolves. In all cases, endometriosis decreases (and usually disappears) after menopause.
However, complications remain possible, including:
- adhesions;
- rarely, pneumothorax, which occurs during menses if lesions are present in the pleura;
- infertility (very common). Usually, it occurs in severe endometriosis.
when lesions reach the peritoneum, ovaries, or fallopian tubes. In fact, it is common for the evaluation related to infertility to reveal endometriosis.
When to start endometriosis treatment?
Starting treatment is recommended only when endometriosis affects daily life or organ function.
To reduce endometriosis injuries that are hormone-dependent and that progress with the menstrual cycle, doctors prescribe drugs that cause menstrual periods to stop (amenorrhea). With no menstrual periods and thus no bleeding from endometriosis lesions, pain lessens or disappears and the lesions regress.
However, some injuries, such as adhesions, endometriomas (located in the ovary), and scarring that is fibrous, are insensitive to hormones and do not regress with this treatment.
Please contact us at http://wa.me//+22967546677
Choice of drugs to treat endometriosis
When determined in consultation with the young woman, it takes into account the contraindications of the drugs, their possible adverse effects, and the person's health status.
First-line hormone therapy
Combined hormonal contraceptives: Some combination hormonal contraceptives used continuously suppress menstrual periods.
Levonorgestrel-releasing intrauterine system (IUD) insertion.
Second-line hormone therapy
Oral microprogestogen contraception with desogestrel.
Etonogestrel implant. It is a long-acting subcutaneous implant that releases a progestin and provides effective contraception.
Chlormadinone acetate (Luteran). The High Authority for Health states that, in the absence of recent data, the place of chlormadinone acetate (Luteran) in the treatment of endometriosis cannot be specified. Tell your doctor if you are taking or have been taking this medicine.
Progestogens Lutenyl and Luteran: warning from the National Agency for the Safety of Medicinal Products
There is an increased risk of meningioma (tumor, most often benign, of meninges, brain and spinal cord envelopes) associated with the use of nomegestrol acetate (Lutenyl and generics) and chlormadinone acetate (Luteran and generics).
Tell your doctor if you are taking any of these medicines.
Gonadotropin-releasing hormone (GnRH) analogs. These drugs prevent the production of gonadotropic hormones, which stimulate the ovaries and thus lower the level of estrogen (hypoestrogenism). This results in the suppression of menstrual periods (amenorrhea) and simultaneously the disappearance of bleeding from endometriosis lesions.
These drugs are prescribed for 3 to 6 months, up to a year. They have side effects—hot flushes, dry skin, bone demineralization, or osteoporosis—related to the hypo-estrogenesis they cause. These are corrected with add-back therapy: a small amount of estrogen is reintroduced into the body, under medical supervision, prescribed before the 3rd month of treatment.
Dienogest (a hormone that acts like progesterone).
Relieving endometriosis pain
Pain management is individualized for each patient and combines hormonal treatments, possibly surgery, and analgesics.
Pain is related to the inflammatory process, irritation of nerve endings, and immobility of tissues in response to pain.
To relieve pain due to endometriosis, doctors prescribe nonsteroidal anti-inflammatory drugs (NSAIDs). Nonsteroidal anti-inflammatory drugs should not be used when contraindicated or for long-term use because of their gastric and renal side effects. If necessary, treatment should follow the following rules and be taken on medical advice:
Use the NSAID at the lowest effective dose.
Do not exceed 5 days of pain treatment.
Discontinue treatment as soon as symptoms resolve.
Other drugs that relieve endometriosis pain include antidepressants used to relieve pain.
Nondrug therapies are often useful to improve quality of life and combat pain, supplementing medical care:
- acupuncture,
- osteopathy (non-manipulative manual therapy, such as fasciotherapy),
- yoga,
- hypnosis.
Please contact us at http://wa.me//+22967546677
Medical Treatment of Endometriosis
SURGICAL TREATMENT OF ENDOMETRIOSIS
Surgery may be needed. It is then programmed in consultation with several specialists: gyneco-obstetrician, urologist (urinary system specialist), digestive surgeon, etc.
This surgery is complex, especially if lesions are implanted on functional organs (bladder, rectum, colon, etc.). Thus, it should be done by surgeons who are experts in endometriosis.
The benefit of surgery is being studied:
in case of painful endometriosis, infertility with desire for pregnancy and depending on the organs affected by endometriosis, provided that the surgery brings more benefits (e.g. reduction of pain, improvement of fertility) than disadvantages (e.g. urinary incontinence);endometrioma (damage to the endometriosis of the ovary).
The procedure begins by taking stock of the extent and nature of endometriosis damage. It then destroys the lesions (by clotting or laser vaporization) or removes them (excision). Surgical difficulty is increased by the presence of small disseminated lesions. Surgery is most often done using laparoscopy, a technique that facilitates surgery and limits adhesions.
If endometriosis is deep or widespread, laparotomy (opening of the abdominal wall) may be needed, and surgery takes a long time. Sometimes removal of a lower digestive tract injury from the rectum requires placement of a stool-diverting bag for 1 to 2 months.
After surgery, hormonal therapy (combined hormonal contraceptives, levonorgestrel-releasing intrauterine system) is used if women do not want to become pregnant to reduce the risk of painful recurrence (if they do not want to become pregnant).
Note: Before surgery, consultation with an anesthesiologist is mandatory.
Please contact us at http://wa.me//+22967546677
MEDICAL MONITORING OF ENDOMETRIOSIS
If you have endometriosis, regular monitoring is indicated throughout your period of genital activity to:
- take stock of any care provided (effectiveness and tolerance) and check that your care is optimal;
- Observe the course of the disease;
Teach you how to live with it better every day.
This monitoring is carried out by the multidisciplinary team that developed your treatment (attending physician, gynecologist, surgeon, radiologist, etc.)
It is based on several consultations and examinations (ultrasound, MRI, etc.), according to a schedule set in consultation with you.
After menopause, symptoms and lesions disappear, this follow-up is staggered or stopped.
You can help make it happen yourself by following a few tips.
Gain a better understanding of your condition by talking to your treating doctor and the specialists who treat you. They will answer your questions and give you personalized advice.
Keep up with scheduled appointments and exams with your team.
Tell your doctor immediately about any unusual or new symptoms that worry you (pain, urinary problems).
When you see a health care professional for another illness, tell them that you are being treated for endometriosis.
For your treatment to be effective, adhere to it and never stop it without medical advice. Tell your doctor about any side effects of the treatment, looking for ways to reduce or prevent them (bone pain, flushing, dry skin, etc.)
SURGICAL TREATMENT OF ENDOMETRIOSIS
Surgery may be needed. It is then programmed in consultation with several specialists: gyneco-obstetrician, urologist (urinary system specialist), digestive surgeon, etc.
This surgery is complex, especially if lesions are implanted on functional organs (bladder, rectum, colon, etc.). Thus, it should be done by surgeons who are experts in endometriosis.
The benefit of surgery is being studied:
- metrioma (damage to the endometriosis of the ovary).
The procedure begins by taking stock of the extent and nature of endometriosis damage. It then destroys the lesions (by clotting or laser vaporization) or removes them (excision). Surgical difficulty is increased by the presence of small disseminated lesions. Surgery is most often done using laparoscopy, a technique that facilitates surgery and limits adhesions.
If endometriosis is deep or widespread, laparotomy (opening of the abdominal wall) may be needed, and surgery takes a long time. Sometimes removal of a lower digestive tract injury from the rectum requires placement of a stool-diverting bag for 1 to 2 months.
After surgery, hormonal therapy (combined hormonal contraceptives, levonorgestrel-releasing intrauterine system) is used if women do not want to become pregnant to reduce the risk of painful recurrence (if they do not want to become pregnant).
Note: Before surgery, consultation with an anesthesiologist is mandatory.
Please contact us at http://wa.me//+22967546677
MEDICAL MONITORING OF ENDOMETRIOSIS
If you have endometriosis, regular monitoring is indicated throughout your period of genital activity to:
- take stock of any care provided (effectiveness and tolerance) and check that your care is optimal;
- Observe the course of the disease
This monitoring is carried out by the multidisciplinary team that developed your treatment (attending physician, gynecologist, surgeon, radiologist, etc.)
It is based on several consultations and examinations (ultrasound, MRI, etc.), according to a schedule set in consultation with you.
After menopause, symptoms and lesions disappear, this follow-up is staggered or stopped.
You can help make it happen yourself by following a few tips.
Gain a better understanding of your condition by talking to your treating doctor and the specialists who treat you. They will answer your questions and give you personalized advice.
Keep up with scheduled appointments and exams with your team.
Tell your doctor immediately about any unusual or new symptoms that worry you (pain, urinary problems).
When you see a health care professional for another illness, tell them that you are being treated for endometriosis.
For your treatment to be effective, adhere to it and never stop it without medical advice. Tell your doctor about any side effects of the treatment, looking for ways to reduce or prevent them (bone pain, flushing, dry skin, etc.)
Discover A very effective Cure to get pregnant in 1 month

